Stop Killing Primary Care
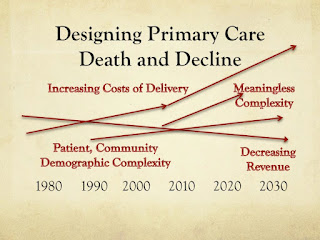
Primary care services have decreased in number steadily, year after year. Payments for primary care services overall have been stagnant as with other basic services taken for granted. Population, demand for care, and complexity are all increasing in ways that should have resulted in much more primary care for anyone who cares about primary care - but there is steadily less primary care. The financial design is broken by stagnant revenue and accelerating costs of delivery. The digital revolution has actually caused regression of primary care via worsening burnout, productivity, and meaningless complexity.
The costs of delivering primary care have been increased across multiple dimensions by those who think that they are improving care when actually they are killing small health, primary care, generalists, general specialties, and basic access to care.
This little death steadily, slowly over time is also specific to primary care physicians who appropriately describe it as trauma similar to PTSD.
Even those that appear to be less burned out have expressed serious concerns regarding the difficulties facing those who deliver primary care.
Death designed from above via finances impacts those below facing the consequences.
The only remaining option for those smaller is to be absorbed by those larger that are paid at higher rates because they are larger. This works if you have attractive locations and patient panels, but not otherwise. And the consequences of being eaten can be significant as those largest often have a different focus - one least understanding of the local, personal, team member, and community aspects of primary care. Care and caring tend to lose when pitted against spreadsheets focused on maximizing revenue and minimizing costs. Then there is the problem that being paid more by moving from small to bigger practice with bigger payment is not likely to change outcomes. This is clearly the opposite of "value-based."
Primary care changes remind us that health care is predominantly about business. The best business models win, the rest lose. The profit focused win. Those focused on the common good of primary care, especially where most needed, lose. Many consider primary care to be important for the common good, but primary care can also be a means to the end of higher profits.
The disruptions of primary care result in opportunities for others - business opportunities, opportunities to make more profits, opportunities to increase market share, opportunities to pay workers less to generate more profits.
Primary care has been undermined by other venues more convenient, those with a better financial design, or both. This worsens the Triple Threat or Deep Squeeze on Primary Care with worsening revenue, higher costs of delivery, and increased complexity.
Others can pick and choose policies and patients and plans that work out best for their finances, leaving the more complex, costly, and burdensome patients to be seen by what remains of primary care practices - especially primary care where most needed.
Time with patients has been disrupted by the design as has time with colleagues, team members, and family of delivery team members. Primary care team members have been disrupted by innovations and regulations resulting in lower productivity and lower revenue generation. Triple Threat Destroys the Essence of Who We Are in Primary Care
Primary care researchers focus their research upon areas that disrupt primary care, while ignoring the disruptions to primary care delivery and the disruptions from quality improvement efforts.
New studies indicate that electronic records are a mismatch with quality improvement, rendering the pay for performance/value based movement the opposite of value.
The designers assumed that software was ready or would adapt. It has never been ready and software corporations have clearly opposed adaptation and necessary support.
Taking the themes from the recent EHR Dysfunction Reports, it is possible to highlight discordance, data issues, unreceptive/unresponsive leadership, and consistent negative impacts upon the practices most important for most Americans left behind.
Discordance
These and other areas indicate primary care services failure by design.
Even family medicine leaders have finally admitted that EHR designers should start over - by quoting those who have designed EHR and failed. This has not ended their support of innovation and regulation as well as contributing to more complexity with their own payment design.
Failure By the Numbers
The costs of delivering primary care have been increased across multiple dimensions by those who think that they are improving care when actually they are killing small health, primary care, generalists, general specialties, and basic access to care.
This little death steadily, slowly over time is also specific to primary care physicians who appropriately describe it as trauma similar to PTSD.
Even those that appear to be less burned out have expressed serious concerns regarding the difficulties facing those who deliver primary care.
Death designed from above via finances impacts those below facing the consequences.
The only remaining option for those smaller is to be absorbed by those larger that are paid at higher rates because they are larger. This works if you have attractive locations and patient panels, but not otherwise. And the consequences of being eaten can be significant as those largest often have a different focus - one least understanding of the local, personal, team member, and community aspects of primary care. Care and caring tend to lose when pitted against spreadsheets focused on maximizing revenue and minimizing costs. Then there is the problem that being paid more by moving from small to bigger practice with bigger payment is not likely to change outcomes. This is clearly the opposite of "value-based."
Primary care changes remind us that health care is predominantly about business. The best business models win, the rest lose. The profit focused win. Those focused on the common good of primary care, especially where most needed, lose. Many consider primary care to be important for the common good, but primary care can also be a means to the end of higher profits.
The disruptions of primary care result in opportunities for others - business opportunities, opportunities to make more profits, opportunities to increase market share, opportunities to pay workers less to generate more profits.
Primary care has been undermined by other venues more convenient, those with a better financial design, or both. This worsens the Triple Threat or Deep Squeeze on Primary Care with worsening revenue, higher costs of delivery, and increased complexity.
Others can pick and choose policies and patients and plans that work out best for their finances, leaving the more complex, costly, and burdensome patients to be seen by what remains of primary care practices - especially primary care where most needed.
Time with patients has been disrupted by the design as has time with colleagues, team members, and family of delivery team members. Primary care team members have been disrupted by innovations and regulations resulting in lower productivity and lower revenue generation. Triple Threat Destroys the Essence of Who We Are in Primary Care
Primary care researchers focus their research upon areas that disrupt primary care, while ignoring the disruptions to primary care delivery and the disruptions from quality improvement efforts.
New studies indicate that electronic records are a mismatch with quality improvement, rendering the pay for performance/value based movement the opposite of value.
The designers assumed that software was ready or would adapt. It has never been ready and software corporations have clearly opposed adaptation and necessary support.
- We already know that financial incentives are not capable of shaping improved outcomes (Annals of IM Comprehensive Review).
- Micromanagement of costs has also been demonstrated by CBO to cost as much as has been saved.
Taking the themes from the recent EHR Dysfunction Reports, it is possible to highlight discordance, data issues, unreceptive/unresponsive leadership, and consistent negative impacts upon the practices most important for most Americans left behind.
Discordance
- between guidelines and measures
- between intention for better quality while worsening access, costs of delivery, disparities, and quality
- between claims of solutions but instead adding to complications, lower productivity, and burnout.
- The designers have never understood the problems facing half of Americans with half enough primary care.
- Focus on overuse has resulting in ignorance regarding vast populations suffering from underutilization - and of course they do not even show up in the data largely collected for billing purposes. Their existence does not show up in billing, reports, state plans, or national plans.
- Data collections have often been limited to the largest and academic practices as noted by MGMA. The Dartmouth Assumptions leading to the ACA design were based on just 20% of the population. (Sullivan about Orsag, Dartmouth, ACA)
- The data collected is insufficient for quality improvement or for assessing important areas such as social and other determinants of health outcomes
- The data cannot even be collected efficiently or effectively or verified
- The designers have failed to supply the necessary revenue and have stripped primary care of what remains. Nurses, teachers, public servants, public health, and others doing the basic person to person services have also been neglected.
- Those that appear to do poorly are blamed when in fact they are doing poorly because they are supported poorly, paid poorly, and are forced to do meaningless uses that erode their core values - service, person to person interactions, care delivery, and caring.
- Larger practices and systems have been unreceptive to primary care for decades. Unrest in primary care physicians and clinicians has resulted in their departure for positions that would do better than pay them for a measly 35 hours while working 55 hours with the stress of 75 hours a week
- The options for small and independent practices and physician autonomy have been terminated by designs and designers acting in concert with insurance payers.
- Software vendors have enjoyed mandates for their products - giving them little reason to invest in a quality product that would actually improve function.
- Articles in journals and in the media are often little more than promotions for innovation, regulation, certification, and digitalization - adding to disruption and dysfunction and discord.
- CMS and insurance payers have been spectacularly unreceptive to the literature, to panels such as MedPAC, and to experts questioning their assumptions
- Foundations and government research efforts and even primary care associations have largely promoted costly, inefficient, and ineffective changes which has been a fit with their needs but at the cost of health access, primary care, cognitive services, office services, generalist workforce, and general specialty workforce - and at the worst possible time with demographic changes and population migrations.
These and other areas indicate primary care services failure by design.
Even family medicine leaders have finally admitted that EHR designers should start over - by quoting those who have designed EHR and failed. This has not ended their support of innovation and regulation as well as contributing to more complexity with their own payment design.
Failure By the Numbers
Primary care services have decreased by 16% for 2016
compared to 2012. This is likely to continue at a 4% decline a year or greater (as in NYTimes and their sources used from Health Affairs and others). Only those so focused on care where care is concentrated can ignore the fact of primary care decline. Even in the state with top concentrations of primary care and other workforce, Massachusetts, there are primary care access issues. Indeed there are segregated pockets of populations lacking access even in the shadow of some of the places with the highest concentrations of US physicians, nurse practitioners, and physician assistants.
There is little doubt that this is due to a seriously flawed financial design and undermining from retail, urgent, emergent, and telehealth. Not only is this bad for primary care, it is worse for the nation due to more fragmentation and services provided without changes in outcomes - the opposite of value.
There is little doubt that this is due to a seriously flawed financial design and undermining from retail, urgent, emergent, and telehealth. Not only is this bad for primary care, it is worse for the nation due to more fragmentation and services provided without changes in outcomes - the opposite of value.
- Retail care estimates of growth range from 7 to 14% annual growth in visits.
- Urgent care is growing at 6% a year.
- Despite these changes, emergency room visits continue to average 2.4% annual growth (ACEP).
Primary care as a proportion of annual health spending is in
decline – despite AAFP goals of doubling primary care spending. As usual AAFP and others cling to false hopes of a better (and more complex) payment design - one that will add to the Triple Threat complexity that continues to damage primary care (revenue, costs of delivery, complexity).
Yes, a few states have mandated insurers to increase primary care
spending, but there is no indication that this can keep up with losses. Sadly these few successes may hide the truth of steady declines from those looking for the optimistic who continue to avoid reality and effective action.
Primary Care Doing Well Is Lowest Value
Primary care is closing, merging, and compromising. The value-based focus was supposed to improve outcomes or decrease costs or both to influence a better ratio defined as higher value. In fact, the opposite is going on. To do well, practices need to be absorbed by those larger and better paid. This can result in revenue generation 20 - 40% higher as practices paid better can support team members better and avoid costly disruptions better. Perhaps the only satisfied primary care physicians are those who have managed to attract and sell their practices or merge them with someone larger and better paid.
But what does this do to value? Obviously paid more for the same services and results is the opposite of value - a move to lower value.
But what is valuable? Meanwhile the practices paid 15 - 20% less for office services often have similar outcomes - clearly top value because of ratios of outcomes to costs as well as serving patients where primary care is half enough - by financial design. Interestingly CMS has dedicated 100 million dollars to a special program to help train existing physicians to move to value-based innovative designs. Instead of supporting these practices threatened with closure, CMS is sending more money to practice consultants to train the most valuable in the hopes that somehow they will adopt value-based designs - the designs that usually result in them paid less for caring for patients with inherently lower outcomes. CMS also denies paying practices more for the care of those who are more complex and inherently have lower outcomes - because this could result in gaming the system.
A Consistent Stream of Innovation Disruption
Primary Care Doing Well Is Lowest Value
Primary care is closing, merging, and compromising. The value-based focus was supposed to improve outcomes or decrease costs or both to influence a better ratio defined as higher value. In fact, the opposite is going on. To do well, practices need to be absorbed by those larger and better paid. This can result in revenue generation 20 - 40% higher as practices paid better can support team members better and avoid costly disruptions better. Perhaps the only satisfied primary care physicians are those who have managed to attract and sell their practices or merge them with someone larger and better paid.
But what does this do to value? Obviously paid more for the same services and results is the opposite of value - a move to lower value.
But what is valuable? Meanwhile the practices paid 15 - 20% less for office services often have similar outcomes - clearly top value because of ratios of outcomes to costs as well as serving patients where primary care is half enough - by financial design. Interestingly CMS has dedicated 100 million dollars to a special program to help train existing physicians to move to value-based innovative designs. Instead of supporting these practices threatened with closure, CMS is sending more money to practice consultants to train the most valuable in the hopes that somehow they will adopt value-based designs - the designs that usually result in them paid less for caring for patients with inherently lower outcomes. CMS also denies paying practices more for the care of those who are more complex and inherently have lower outcomes - because this could result in gaming the system.
The system is clearly gamed - for those largest and against those most needed.
A Consistent Stream of Innovation Disruption
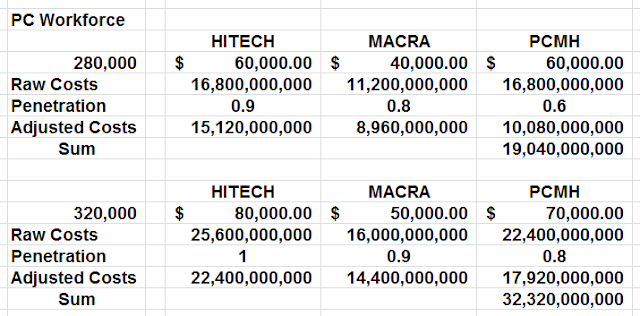
Primary care has had to subtract 19 to 32 billion dollars to address HITECH to ACA to MACRA to PCMH. These are not the only higher cost areas that have been forced upon lowest paid and least supported primary care.
180 billion minus 32 billion leaves 148 billion
to invest in
primary care delivery
You cannot do with 148 billion what you once did with 180 billion. You cannot have as many team members or be as comprehensive or keep patients satisfied or team members for that matter. Only the primary care that has multiple sources of support or has the advantage of the best plans and patients can do well.
Thin margins existed a decade ago. What value is there in 11% to 16% of revenue forced out of practices and communities in most need of these billions. "Innovation" and regulation have clearly done a number on primary care.
And of course where primary care has been and remains half enough, expansions of insurance have little impact, particularly for the public and private plans that pay less than margin or do not pay at all (high deductible) where small health care is dominant and dying by design. The real problem all along for these areas was lack of workforce impairing access for insured and uninsured alike. They actually had insurance levels at the national average. Their problem was the worst public and private plans. Their problem also remains the worst social determinants - limiting health care finances and outcomes under the US designs.
But Wait, the Cost of Delivery Increases Are Even Greater
Other costs have increased in the usual areas. Worsening cost areas include the increasing costs of turnover - recruitment, retention, locums, brokers, orientation costs, and lost productivity. These have reached $100,000 per primary care physician lost per year or $300,000 per physician with physicians lasting less than 3 years. The actual cost added annually over the past decade is in likely closer to 40 billion subtracted now compared to ten years ago or easily 20% although as noted some advantaged primary care practices are doing better while disadvantaged have been forced to close, compromise, or downsize in the face of increasing need.
Designs Dictate Who Wins and Who Loses
The obvious gains in primary care budgets are seen for software, hardware, HIT, EHR, security, costs for adapting to EHR, consultants, managers, associations preparing practices, and more people to manage insurance and regulations. Those who benefit from micromanagement of cost and micromanagement of quality gain while primary care delivery loses.
Both micromanagements are shown to fail.
- The costs for micromanaging costs are higher – eating up any savings (CBO reports) while disrupting
- The so-called “quality” outcomes are not influenced by financial incentives as demonstrated in evidence based reviews and as noted by various experts (Annals IM, Casalino, Sullivan, Soumerai, others)
- The payment designs based on incentives (pay for performance, value based, readmissions penalties) have been shown to discriminate against those delivering care where needed (same sources) where patients are older, sicker, and have lesser social determinants - real determinants of outcomes (Hong in JAMA, Sullivan, others)
- Business practices also result in lesser costs due to discounts for those larger and most organized with greater costs of delivery for those smaller in areas such as supplies and other payables
- Payer practices result in higher payments for those larger and most organized with lesser payments and the fewest lines of revenue for those smaller. Big insurance is massive compared to those small. Big vs small is a killer for smalls.
As many have noted, once a cycle of decline has started with the loss of one or more physicians or clinicians, a small practice may have difficulty recovering. Clearly some most familiar with this design have closed practices or moved out.
Revenue issues, cost of delivery increases, meaningless complexity increases, demographic complexity increases - over and over...
So Why Do Family Medicine Organizations Support Decline by Design?
All the above are made worse where family physicians are found as they are 3 times more likely to be found where primary care services are paid less by 15%. This is such great treatment for those who most contribute to access where access is lesser or absent. It is a wonder that we have access at all for most Americans with declines across primary care, mental health, women's health, general orthopedics, general surgery, and other general surgical careers for over a decade.
All the above are made worse where family physicians are found as they are 3 times more likely to be found where primary care services are paid less by 15%. This is such great treatment for those who most contribute to access where access is lesser or absent. It is a wonder that we have access at all for most Americans with declines across primary care, mental health, women's health, general orthopedics, general surgery, and other general surgical careers for over a decade.
Revising Standard Primary Care Year Estimates
My studies dating back a decade regarding the Standard Primary Care Year demonstrated stagnant primary care workforce with a slight growth projected. The Standard Primary Care Year predicted primary care delivery of a graduate at the year of graduation based on retention, activity in practice (lower for NP, PA, IMG), years in a career (21 for NP, 33 for others), and volume adjustment (lower for NP and PA). I multiplied this contribution by the number of graduates in each class year.
I was incorrect in my assumptions of retention regarding primary care sources – especially family medicine. Declines in retention have proceeded rapidly. It took some time for the Graham Center and others to indicate the substantial losses of family physicians away from office family practice with increases in ER to 12%, urgent to 4% and hospitalist to 4% a decade ago and the losses are worse and now involve more areas.
New Standard Primary Care Year projections would indicate a
decline in capacity despite massive expansions in all four sources (MD DO PA and especially NP) because of lower retention than
projected in NP, PA, and FM.
Changes in activity in females and males as well as better opportunities outside of primary care reduce the primary care delivery capacity for each graduate of each source and shape more to retail, urgent, emergent, hospitalist, and subspecialist careers. Others leave health care for better opportunities outside of care delivery.
Changes in activity in females and males as well as better opportunities outside of primary care reduce the primary care delivery capacity for each graduate of each source and shape more to retail, urgent, emergent, hospitalist, and subspecialist careers. Others leave health care for better opportunities outside of care delivery.
Declining Primary Care By Source
The internal medicine declines in entry and retention have
resulted in replacement by other sources other than pediatrics. This has long
been known. IM has collapsed from 150,000 down to less than 30,000 in the next
few years. Internal medicine once contributed generalists that were 13% of workforce in lowest concentration counties and about 30% of local primary care. The future is less than 5% of local workforce where needed and perhaps 10% of local primary care. Schools rich in internal medicine production are poor in primary care and care where needed.
PD workforce has demonstrated stagnation as graduates have increased from 1400
to 2100 a year but the pediatric office result remained the same due to declines in retention - another indication of insufficient dollars for primary care involving pediatrics - particularly the public plans.
The roads all point the same way but the mapmakers cannot read the map.
MPD is not significant in numbers especially when correcting
for retention and the fact that MPD morphs into the above two.
The collapse of family medicine was not anticipated
I assumed 85% active in family medicine. This was true in the 1970s and early 1980s graduates but the declines have been steady. Appropriate studies by primary care researchers would have identified this and might have been done, but it apparently took time for the truth to get released.
It is likely that only 50% of FM grads will be retained in office primary care for the most recent graduates. As with other sources of primary care, family medicine associations will soon have less than a majority involved in primary care. Lack of consideration for primary care, especially primary care where needed, is already a major concern. Any real concern would have resulted in a strong and steady fight against the rapid increases in costly disruptions, innovations, and regulations.
The Graham Center previously announced levels of about 76,000 family medicine residency graduates who were in office FM. This compares to 3000 x 35 years or about 105,000 who could practice – but the levels are more like 55,000 to 60,000 now and are declining
I assumed 85% active in family medicine. This was true in the 1970s and early 1980s graduates but the declines have been steady. Appropriate studies by primary care researchers would have identified this and might have been done, but it apparently took time for the truth to get released.
It is likely that only 50% of FM grads will be retained in office primary care for the most recent graduates. As with other sources of primary care, family medicine associations will soon have less than a majority involved in primary care. Lack of consideration for primary care, especially primary care where needed, is already a major concern. Any real concern would have resulted in a strong and steady fight against the rapid increases in costly disruptions, innovations, and regulations.
The Graham Center previously announced levels of about 76,000 family medicine residency graduates who were in office FM. This compares to 3000 x 35 years or about 105,000 who could practice – but the levels are more like 55,000 to 60,000 now and are declining
The declines have long outpaced growth of annual graduates.
FM has had a paltry 1% average growth of annual FM grads since 1980. Yes, the
only real expansion was provided by the original financial designs and the
original FM leaders who moved into leadership from their practices (not the same
as the academic leaders taking the reins since 1980). Yes, the only real expansion
of FM from 1970 to 1980 to the level of 3000 annual graduates occurred when FM
had 5 main things going for it
1. No
competition for broad scope
2. Massive
expansions of funding 1965 to 1978 via Medicare and Medicaid – steady increases
in annual fee payments were also seen
3. Funding
specific to elderly and poor and basic services in the initial design
4. Relatively
lower cost of delivery increases
5. Better
economics in areas lowest in concentrations of physicians – manufacturing,
mining, agriculture, government positions (agriculture, forestry, environment)
combined with less foreign competition
That was then, this is Now.
1. Now there is
competition for broad scope which is actually reduced
2. Expansions of
funding have long ago ended and revenue has been lost due to losses of Ob,
hospital, ER, assistant surgery, and other services – also revenue is declining
by innovative design and higher turnover
3. Funding has
been moved far beyond basic services to procedural, technical, subspecialized
with less pay for primary care and primary care where needed – deaths of small
hospitals and small practices
4. Accelerating
costs of delivery in multiple dimensions – patient demographics,
micromanagement of costs (referrals, approvals, reports, delays, denials),
micromanagement of outcomes, innovations, digitalizations, certifications,
regulations, insurance, supplies
5. Worse
economics in areas lower in concentrations of physicians across the board with
worse to come in each area plus areas such as declines in SNAP, Social
Security, Disability, and other funding that has had equitable distribution
Back to Review of Sources continuing with NP – Essentially
there is a rearrangement of the deck chairs of the Titanic with stagnant to
declining finances shaping stagnation in primary care, rural health, and lowest concentration
county care. New sources can replace the old, but can not increase delivery
capacity. But still there are those on the sidelines that claim that they can be a solution (pharmacy associations, assistants made out of physicians from other nations). If you advocate for these groups or consider training to be the problem, then you will promote your solution but this does not address the financial failure resulting in primary care failure.
Massive Expansions Have Failed
Massive Expansions Have Failed
Massive Expansions Have Failed
Massive Expansions Have Failed
NP graduates continue to grow at about 12 times the level of
annual US population growth – blasting past 26,000 two years ago and increasing
at 1300 to 1600 a year still. Massive expansions of NP PA DO Caribbean and MD
have not improved any real shortages.
Massive expansions of NP and PA graduates have been able to cover for some of the IM and FM
losses, but result in the least experienced workforce as turnover is much
higher and fewer remain in the same primary care practices and departures
outside of primary care are also higher.
(Do the calculations – Primary care at 3500 to 5000 a year for decades
as a workforce moving to those with least hands on training and perhaps 1500 to
2000 annual visits narrow in scope and not supervised – services done by those
planning their escape from the practice or from primary care almost as soon as
starting.)
PA expansions are growing at about 8 – 10 times annual
population growth and studies demonstrate essentially no gain in primary care
with each doubling. The primary care result has been cut in half. New graduate
studies demonstrate a 30% increase in primary care with a 100% increase in
annual graduates and a 200% increase in non-primary care result. The 30% added
to primary care are essentially gone within a decade as these transition away also.
NP and PA also have more in part time. NP has more preparing
for their next career, shorter careers of 20 years, more between jobs, and 40%
of those who could practice choose not to practice as with RN graduates. NP is
96% female according to federal occupations census data.
DO doublings have also resulted in no primary care gain as
the family practice result, the predominant DO primary care result, has been
cut in half. The Pandora’s Box of GME consolidation has opened up many more
options for DO graduates which will decline family practice in favor of
flexible primary care or non-primary care choices.
IMG losses are 20 – 40% who never do US practice and
retention is lower in primary care and any distribution benefits are lost after
a few years – for those who remain in the US and remain active
Bigger Most Organized Win and Most Lose
By the way, the federal shortage designation process does not
actually reflect shortages as systems and practices refusing to serve Medicaid
allow highest workforce concentration areas to get shortage area funding. All
you need to do is work with the health department to document this – which is
what large systems and academic systems often do. This is why regulations were
needed to retain 20% of such funding for rural areas (although they should get
at least 30% due to higher need). Three attempts to reform the design have failed. Dollars go to those most organized and doing best while others fall behind.
Those largest and most organized can figure out any and all
ways to get all lines of revenue and the most reimbursement or benefit from
each line.
Those smaller, least organized, more distant, and most
needed have no voice – indeed the health care leaders have little clue about
this situation and how associations, institutions, and foundations have made
this much worse by do-gooder approaches that add to disruptions and decrease
productivity.

This comment has been removed by a blog administrator.
ReplyDeleteThis comment has been removed by a blog administrator.
ReplyDeleteGood Work Go Doc Web
ReplyDeleteI adore your websites way of raising the awareness on your readers. website here
ReplyDelete