Who Really Benefits?
In past Basic Health Access blogs, claims of benefit to health access have been pointed out as promotions and promises, impractical, deceptive, or insignificant. Over and over the design deficits do not allow health access recovery. Most of these assertions and assumptions and promotions fail as they simply ignore massive and increasing shortages of the best and most experienced and most committed basic health access professionals – by far the most pressing need for basic health access for the next 20 years and likely longer.
The US simply does not have a design for training and for supporting the workforce needed for over half of Americans.
Past blogs have indicated that claims of benefit for rural areas or underserved areas are not entirely true as the real benefits go to academic institutions, software companies, or others who help themselves by the design. Foundations appear to be innovative and cutting edge by recommending new types of primary care despite the fact that these types are 3 to 1 not primary care in result.
Some foundations fueled by the billions going to health insurance corporations (such as United Health Care) appear to be promoting types of workforce that undercut physician workforce – a sure way to create more easily controlled health professionals - centralizing control in the hands of fewer and those most distant from care delivery. Sadly designs have already been implemented that will result in massive excesses of non-primary care led by 70 - 80% of nurse practitioners and physician assistants found in non-primary care areas. Massive expansions without real focus are a sure way to increase health care costs and more profits for health insurance companies, academic institutions, and large systems - those that benefit most from non-primary care excesses and ever higher costs with more subspecialized care.
Innovation and reorganization appears attractive during periods of desperation, but fixing desperation is about fixing designs that result in failure - not more innovation and especially not more innovation that proceeds from those that shape failed designs. All else tends to fail because of the policy design. Pipelines worked when policy worked but then failed when policies failed. Innovation and reorganization could work with a better design, but cannot work without a better policy design. No design can work without the workforce to serve where needed as this shapes health spending, health access, and distributions of health spending. Ever greater focus on innovation and reorganization is not the correct approach.
The one type of primary care that predates all new types has the best primary care retention and the best distribution in the most important category – delivery of primary care where needed as measured over an entire career of workforce contribution. The broadest generalist primary care workforce is always the solution for health access as long as it remains broadest generalist over an entire career. Family medicine existed before the innovations, got better because of the formalization of family medicine training, has remained most valuable for the past 40 years of family medicine's existence, and still contributes the most to primary care, to rural health, to care in underserved locations, and to local health care for 30,000 zip codes with 65% of the population and increased proportions of all in most need of care. Family medicine is also the one type of health access that has not been expanded in 30 years because so few under current policy will make a permanent choice of primary care most likely to be found where the US design sends the least spending.
Any evidence based focus on health access would see this as designers of US health care actually avoiding health access interventions such as family medicine that have worked for far more than the past few decades.
Readers are invited to review the following link and decide for themselves if Alabama, Kentucky, Arkansas, the Mississippi Delta, or other rural areas will really benefit, or whether the funds will go for someone else’s purposes (beyond the political desires of whatever administration is current). Year after year, administration after administration, Congress after Congress, we see the same news releases – but we continue to fail in basic health services despite spending far too much money upon health.
Agriculture Secretary Vilsack Announces Funding to Improve Access to Health Care in Rural Areas Nov 21, 2011 -- Agriculture Secretary Tom Vilsack last week announced funding to establish telemedicine and other health care projects to address unmet health care needs in the Delta region.
I have learned to examine these various claims of benefit to see who benefits. This is another in a long and glorious tradition of political claims that fail in specific benefit to those most in need.
Will Arkansas, Illinois and 48 other states keep pouring millions into pre-health programs that fail to result in return in investment given only 1 out of 3 that actually make it to admission and less than 1 out of 5 that may serve in some needed career or location? Perhaps states will finally figure out that they should obligate MD, DO, NP, PA, and RN students at admission to train for needed health access locations – as a condition of admission. Then funding at each of 7 different levels is of little consequences since at least 90% will serve the first 25% of their careers where health professionals are needed – instate in locations in need. This is a far cry better than medical schools that attempt partial pipelines where only 1 in 8 graduates are found where needed, and mostly because they chose family medicine. A major advantage known for training is trainees that prepare for their careers all of the years of training. When trainees exhibit this (rural family medicine, pediatrics) or are obligated for these careers, they will better prepare themselves for such careers because their pathway was known from the start. See Addressing the Primary Care Crisis.
Does $700,000 for interlinked rural intensive care units work, or perhaps would $700,000 mobilize resources to attack maternal obesity in Mississippi - a condition that kills at least 4 youngest mothers a year across the state? Will these rural hospitals even survive the next 5 years of cuts? Will any intervention help when our nation divides further into richer and poorer – the reason for increased stressors especially in those most left behind and the reason for increased food consumption and other adverse behaviors resulting in poor maternal outcomes long before pregnancy?
I have to admit that linking rural sites is a good idea as in Project Echo in New Mexico, but will this project have a Dr. Sanjeev Arora and the U of NM and public health driving collaborative two way access. Project Echo in New Mexico focuses on delivering care to people in need of care – not stroke. The benefits are also better trained primary care professionals on the front lines. Another benefit is far fewer specialists needed with more primary care supported where needed rather than the current design that steadily collapses all health workforce toward 1% of the land area.
Is it helpful to pay 3 million dollars to have an urgent care center in Mound Bayou? Is this expenditure a measure of the failure of one of the first Community Health Centers in the nation to actually work? Why not primary care or CHC offices open until 8 or 9 PM? Was there no ER willing to branch out and if not, perhaps the reason was the lack of health care coverage or sufficient available local health spending? If the area was unable to sustain urgent care for 80 miles, does it need urgent care? Will 3 million dollars as a one time expenditure prop up an urgent care that is not viable under the existing design? Will the urgent care have the workforce needed or will it steal local primary care workforce and compromise local primary care? Can urgent care paid multiple times more for the same services help a region short on cash, short on workforce, and short by US design?
Then there is this political announcement:
“Since taking office, President Obama's Administration has taken historic steps to improve the lives of rural Americans, put people back to work and build thriving economies in rural communities.”
Should we be impressed after 30 years of such press releases?
Do the examples of a few rural locations mean anything in a sea of shortages caused by designs for elsewhere? Can centralized designs shaped by those most centralized really help locations that require decentralized training, workforce, and spending? There will never be enough in any special program to help rural areas, underserved areas, and most Americans in need of basic health services. Total failure is the result of poor designs that have totally failed. Double or triple or quadruple the special program spending would not help. The across the board cuts directly or indirectly or relative over decades will make matters worse for areas that need more spending, not less. The designers can use delay tactics and can confuse only if we let them. Real designs for health and for health care are needed.
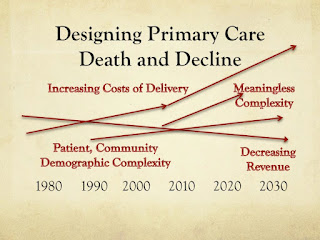
For 30 years administration after administration has failed to distribute health spending and health workforce that would truly improve the lives of rural Americans as well as stimulate jobs and “thriving economies” in rural America. Each 15 years the designs can be traced as sending ever more spending to facilities not found in rural locations in need, sending ever more spending to non-primary care least seen in rural locations, and sending ever more spending to settings with the most health spending already.
Designs for 30 years that are cost cutting in nature, rather than designs for health or health care, are not good for most Americans. The designs leave 70% of rural Americans behind due to marginalization of family practice and primary care and health access. Only rural locations that have managed to replicate the largest urban system designs thrive because they find their way to all lines of revenue and the top reimbursement in each line - and have lowest percentages of primary care and family medicine by design.
Designs that favor those who already have the most workforce and the most lines of revenue and the highest level of reimbursement in each line fail most Americans left behind who have the fewest lines of reimbursement and the lowest levels of reimbursement (rural hospitals, primary care) as well as the least workforce and least economics from health care – by design.
But the media releases, major journal articles, academic planning, accountant-led cost cutting measures, and government reports will all continue. Perhaps one reason is that we all grasp at straws held out. As long as we believe that we can keep our own special programs intact and fund them at ever higher levels we will keep grasping at straws - and will delay real improvements. Financially, politically, and practically it is not possible to hold on to special programming, but we persist.
What we must do to actually resolve so many deficits for most Americans is to work together on a real design based on health and health care down to the local level.
Instead we have spending concentrated in disease focus, concentrated in too few locations, and concentrated on too few for too little result. Also we have the resultant cost cutting design in consequence and too little spent on most Americans in nearly all zip codes.
The Squeeze Play That Fails
How the Disease Focused Abuse Health Access
Deifying Disease By Design
Can We Have Our Billions Back Please?
Exploring the Health Consequences of Disease Focus
How the Disease Focused Abuse Health Access
Deifying Disease By Design
Can We Have Our Billions Back Please?
Exploring the Health Consequences of Disease Focus
Thanks to all 12,000 who have visited Basic Health Access in 2011.
Robert C. Bowman, M.D. Basic Health Access Web Basic Health Access Blog
Dr. Bowman is the North American Co-Editor of Rural and Remote Health and a Professor in Family Medicine at A T Still University School of Osteopathic Medicine. He was the founding chair of the Rural Medical Educators Group of the National Rural Health Association, he was the long term chair of the STFM Group on Rural Health, he is the founding director of Priority Infrastructure at http://www.infrastructureamerica.org/ and he is the author of the World of Rural Medical Education, and Physician Workforce Studies
Comments
Post a Comment