The Deep Squeeze Financial Design Killing Health Access
As an academic family physician specializing in basic health access, I worked to resolve shortages and improve access to care. It was my privilege to work in some of the few remaining schools devoted to such efforts. Sadly this professor found that he was learning impaired - or perhaps I was indoctrinated by the process of medical education. The financial design was far too powerful to allow training design to address deficits.
What appeared to work in the 1965 to 1980 period of time, worked because of the financial design. Each year more dollars were pumped into basic services - especially where poor Americans and seniors were found. As it turns out, these are the areas with the most deficits. Initially the original Medicare and Medicaid designs helped, but they were changed into vehicles to concentrate dollars - not distribute care. The same designers continue to shape the designs into more for few and fewer for more - and basic health access suffers most by design.
My solo rural practice actually taught me all that I needed to know to be able to finally understand the persistent and worsening shortages. During the 1980s, the designs changed from supportive of health care delivery to cost cutting in focus.
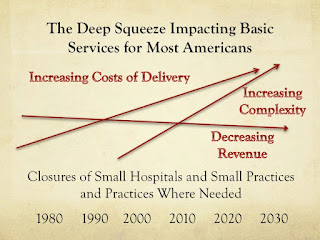
My practice taught me all that I needed to know about the Deep Squeeze or Triple Threat preventing health access - payments too low, costs of delivery worsening, and complexity of practice increasing in multiple dimensions.
This Deep Squeeze
...keeps basic workforce at half the needed levels in places where demand is increasing and workforce is not.
Contributing to the Deep Squeeze
Runaway health care costs from 1980s to the present and beyond have shaped the current health policy era known as the Era of Cost Cutting.
Few if any consider health care, any health care area, worthy of investment including primary care, women's health, mental health, or care where shortages exist.
Distractions Prevent Recognition of Financial Failure
Magical thinking continues to shape false beliefs - particularly the false belief that training can address shortages. This magical thinking only benefits those who train such graduates and receive their tuition dollars along with the financial institutions who add to the debt and the ability to increase tuition dollars.
Despite decades of persistent shortages and the consequences of massive expansions, the expansions of MD DO NP and PA graduates continue at 6 to 12 times annual population growth. Deans, program directors, workforce researchers, and others clamor for more graduates - especially more of their kind of graduate. They have lost touch with the reality. They are actually setting up their graduates of all kinds for the worst situation that can face workforce - too many for too few positions.
Even worse, Americans are being set up for more Runaway Health Care costs. Expansions during the Deep Squeeze can only result in more expensive workforce and more costly and most highly specialized care.
This massive expansion cannot resolve shortages that are fixed in place by stagnant to declining finances. Stop the Insanity of Expansion
The Deep Squeeze Discriminates By Design
New waves of runaway costs leave even more Americans behind. Each new permutation of innovation adds to the costs and complexities of the Deep Squeeze. Those biggest, most organized, and costing the most deflect the cost cutting - resulting in adverse impacts upon
The Deep Squeeze Shapes Burnout and Red Zone Specialties
Basic services are about people serving people. The Deep Squeeze impacts of greater administrative and meaningless costs puts the Deeper Squeeze on personnel - the most costly component of people serving and caring for people. The squeeze is placed upon what matters most to patients, practices, and practitioners. Generalists and General Specialties are clearly targeted by the Deep Squeeze.
We do not need another conference or seminar or practice consultant to address Burnout - the Deep Squeeze Design must be fixed. Who can afford to go to a Burnout Conference when this decreases revenue and increases costs of delivery plus the increased complexity of catching up after a week away to relax and recover?
Those that say that they are devoted to health access such as The Commonwealth Foundation and AAFP should devote all resources to fighting The Deep Squeeze. But we obviously have a failure in perspective. Those devoted to health access have been too involved in innovation and rearrangement as a solution - rather than the most essential component - investments in the people that invest in people. They do not even see that their promotions make costs of delivery and Deep Squeeze worse. Even the basic fight for payment equity has not been made, hitting family practice most of all where family practice is most needed by most Americans.
This Deep Squeeze or Triple Threat destroys the essence of who we are - people serving people.
Design after Design Sinks Health Care and Caring. Only those who have lost touch with the people delivering health care could continue to make matters so much worse with the Deep Squeeze. Fewer are focused upon delivery as a result - and more are focused on profit.
The Deep Squeeze will not allow anything other than a rearrangement of the deck chairs as the concentrations as seen in basics such as primary care remain about 40 - 50 per 100,000 - or half enough for these complex settings due to higher levels of elderly, poor, mentally ill, smokers, and Americans with obesity, diabetes, COPD, and other adverse diseases situations, and environments. This greater complexity not only reflects the challenges of the primary care practices serving most Americans most behind - but this complexity is increasing nationwide due to demographic changes and also due to meaningless use. Even with studies demonstrating the failure of pay for performance and financial incentives and even with studies demonstrating the discrimination of these payment designs - they continue their Deep Squeeze actions.
What appeared to work in the 1965 to 1980 period of time, worked because of the financial design. Each year more dollars were pumped into basic services - especially where poor Americans and seniors were found. As it turns out, these are the areas with the most deficits. Initially the original Medicare and Medicaid designs helped, but they were changed into vehicles to concentrate dollars - not distribute care. The same designers continue to shape the designs into more for few and fewer for more - and basic health access suffers most by design.
My solo rural practice actually taught me all that I needed to know to be able to finally understand the persistent and worsening shortages. During the 1980s, the designs changed from supportive of health care delivery to cost cutting in focus.
My practice taught me all that I needed to know about the Deep Squeeze or Triple Threat preventing health access - payments too low, costs of delivery worsening, and complexity of practice increasing in multiple dimensions.
This Deep Squeeze
...keeps basic workforce at half the needed levels in places where demand is increasing and workforce is not.
Contributing to the Deep Squeeze
Runaway health care costs from 1980s to the present and beyond have shaped the current health policy era known as the Era of Cost Cutting.
Few if any consider health care, any health care area, worthy of investment including primary care, women's health, mental health, or care where shortages exist.
Distractions Prevent Recognition of Financial Failure
Magical thinking continues to shape false beliefs - particularly the false belief that training can address shortages. This magical thinking only benefits those who train such graduates and receive their tuition dollars along with the financial institutions who add to the debt and the ability to increase tuition dollars.
Despite decades of persistent shortages and the consequences of massive expansions, the expansions of MD DO NP and PA graduates continue at 6 to 12 times annual population growth. Deans, program directors, workforce researchers, and others clamor for more graduates - especially more of their kind of graduate. They have lost touch with the reality. They are actually setting up their graduates of all kinds for the worst situation that can face workforce - too many for too few positions.
Even worse, Americans are being set up for more Runaway Health Care costs. Expansions during the Deep Squeeze can only result in more expensive workforce and more costly and most highly specialized care.
This massive expansion cannot resolve shortages that are fixed in place by stagnant to declining finances. Stop the Insanity of Expansion
The Deep Squeeze Discriminates By Design
New waves of runaway costs leave even more Americans behind. Each new permutation of innovation adds to the costs and complexities of the Deep Squeeze. Those biggest, most organized, and costing the most deflect the cost cutting - resulting in adverse impacts upon
- Those smallest
- Those least organized
- Those delivering the majority of services (55%) in primary care
- Those delivering generalist and general specialty services that are 90% of the local services for the 2621 lowest concentration counties (40% of the US) and the zip codes with least access (10 - 20% of the US population)
The Deep Squeeze Shapes Burnout and Red Zone Specialties
Basic services are about people serving people. The Deep Squeeze impacts of greater administrative and meaningless costs puts the Deeper Squeeze on personnel - the most costly component of people serving and caring for people. The squeeze is placed upon what matters most to patients, practices, and practitioners. Generalists and General Specialties are clearly targeted by the Deep Squeeze.
Those that say that they are devoted to health access such as The Commonwealth Foundation and AAFP should devote all resources to fighting The Deep Squeeze. But we obviously have a failure in perspective. Those devoted to health access have been too involved in innovation and rearrangement as a solution - rather than the most essential component - investments in the people that invest in people. They do not even see that their promotions make costs of delivery and Deep Squeeze worse. Even the basic fight for payment equity has not been made, hitting family practice most of all where family practice is most needed by most Americans.
This Deep Squeeze or Triple Threat destroys the essence of who we are - people serving people.
Design after Design Sinks Health Care and Caring. Only those who have lost touch with the people delivering health care could continue to make matters so much worse with the Deep Squeeze. Fewer are focused upon delivery as a result - and more are focused on profit.
The Deep Squeeze in Access
- Is Shaped By the Deep Squeeze in Primary Care
- Is Shaped By the Deep Squeeze in the Financial Design
- Prevents any training design from resolving access woes
The Deep Squeeze will not allow anything other than a rearrangement of the deck chairs as the concentrations as seen in basics such as primary care remain about 40 - 50 per 100,000 - or half enough for these complex settings due to higher levels of elderly, poor, mentally ill, smokers, and Americans with obesity, diabetes, COPD, and other adverse diseases situations, and environments. This greater complexity not only reflects the challenges of the primary care practices serving most Americans most behind - but this complexity is increasing nationwide due to demographic changes and also due to meaningless use. Even with studies demonstrating the failure of pay for performance and financial incentives and even with studies demonstrating the discrimination of these payment designs - they continue their Deep Squeeze actions.
Studies indicate the horror of the Deep Squeeze as
- Primary care physicians spend more time with charts than patients.
- Discrimination in payment design shapes shrinking general specialty workforce and greater decline where concentrations of workforce are least - for worsening access.
- Six Degrees of Payment Discrimination continue to impair care for most Americans by design.
- Micromanagement manipulations from outside steal creativity, time, and caring inside of practices.


This comment has been removed by the author.
ReplyDeleteThank you for sharing. Looking forward and reading more of your blogs!
ReplyDeletehttps://www.copperutensilonline.com/
This comment has been removed by the author.
ReplyDeleteThanks
ReplyDeleteHttp://labellaviecool.blogspot.com/